Aetiology
Urethritis, or inflammation of the urethra, is a multifactorial condition which is sexually acquired in the majority of (but not all) cases.
As per the table below, the commonest organisms implicated are C. trachomatis and M. genitalium. These are most likely to be detected in younger patients, those with urethral discharge and/or dysuria. However, in 30-80% of NGU cases, neither organism is detected.
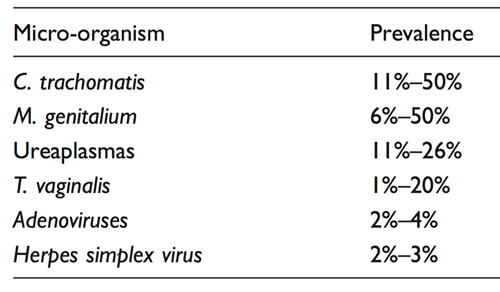
Pathogen negative NGU is more likely with increasing age and the absence of symptoms. Trichomonas vaginalis detection is dependent on prevalence in the community. Other more uncommon causes include urinary tract infection, adenovirus, herpes simplex viruses.
It is recommended that asymptomatic men are not tested for NGU.
Clinical Features
Symptoms
- Urethral discharge
- Dysuria
- Penile irritation
- Urethral discomfort
- Nil
Signs
- Urethral discharge
- Balano-posthitis
- Nil
Complications
- Epididymo-orchitis
- Sexually acquired reactive arthritis / Reiter’s syndrome (<1%)
Diagnosis
Only symptomatic patients and/or those with a visible discharge or presence of balano-posthitis should be assessed for the presence of urethritis (IV, C).
Microscopy
- The diagnosis of urethritis should be confirmed by demonstrating five or more PMNLs per high power (x1000) microscopic field (averaged over five fields) on a smear obtained from the anterior urethra
- Sampling with a 5-mm plastic loop or cotton tipped swab which should be introduced about 1cm into the urethra. A 5-mm plastic loop is less painful than a Dacron swab which is less painful than a Rayon swab (Ib, A)
- If urethral discharge can be sampled without insertion into the meatus, this is recommended but has not been compared to standard technique (IV, C)
- The optimum time between passing urine to urethral smear to ensure a definite diagnosis in a symptomatic man is not known but 2–4 hours is conventional (IV, C).
- As centrifuges are not routinely available to spin urine, a first pass urine may be examined for threads and these Gram-stained and interpreted for a spun deposit (III, B)
Other tests
- All patients should be tested for N. gonorrhoeae and C. trachomatis. Tests for M. genitalium and U. urealyticum are currently not widely available in the United Kingdom
- Testing male patients with urethritis for M. genitalium (and for macrolide resistance if detected) would be helpful in management and should be performed if available
- Test for UTI if clinically indicated
If microscopy is not available:
Patients should be referred to a service providing microscopy, but urethritis may be diagnosed by:
- The presence of a mucopurulent or purulent urethral discharge on examination
- >/1+ on a leucocyte esterase dipstick on an FPU specimen
- The presence of threads in a FPU specimen. Threads may be physiological e.g. semen (IV, C)
Investigation of symptomatic patients with a negative urethral smear
- Leucocyte esterase dipstick on FPU does not have adequate sensitivity and is therefore not recommended for diagnosis in a level 3 service where microscopy is available.
- Patients with negative smears may be reassured and return for early morning smear if symptoms do not settle. It is good practice to advise the patient to take their last drink about 8p.m. and to void about 3 hours later in order to help avoid waking with a full bladder (IV, C)
- Empirical treatment is not recommended (IV)
Management
The Treatment Guidelines were updated in December 2018. Please find below the recommendations of the May 2018 update (or click here). The original recommendations of the 2015 Guideline are also reproduced below.
Update to the 2015 BASHH UK National Guideline on the management of non-gonococcal urethritis
Dec 2018
Up to 25% of uncomplicated cases of non-gonococcal urethritis (NGU) are caused by infection with Mycoplasma genitalium (Mgen). This organism is likely to be implicated in an even higher proportion of cases of recurrent or persistent NGU. However, many men with Mgen infection will not develop NGU.
Optimal management of NGU requires testing for Mgen in addition to C. trachomatis, and providing appropriate antimicrobial therapy in the presence of a positive test (and carrying out a test-of-cure if necessary). The prevalence of pre-treatment macrolide resistance in Mgen in the United Kingdom is almost certainly >40%, which is probably due to the widespread use of azithromycin 1g to treat STIs and the limited availability of diagnostic tests for Mgen.
Pending widespread availability of Mgen detection assays, the Clinical Effectiveness Group has considered the best available evidence and updated the NGU guideline so that treatment regimens are consistent with the revised chlamydia and the new Mgen guideline.
Treatment of First Episode NGU
Recommended
Doxycycline 100mg twice daily for 7 days
Alternatives
Azithromycin 1g stat then 500mg once daily for the next 2 days (three days total treatment)*
NB Patients should be advised to abstain from sexual intercourse until 14 days after the start of treatment, and until symptoms have resolved. This is likely to reduce the risk of selecting/inducing macrolide resistance if exposed to Mgen or Neisseria gonorrhoeae which would make these infections more difficult to treat.*
or
Ofloxacin 200mg twice daily, or 400mg once daily, for 7 days
*While there are no data on the utility of this regimen in treating NGU caused by Mgen without pre-existing macrolide resistance mutations, it will be at least as effective as 500mgs then 250mgs once daily for the next four days for which there is moderate but conflicting data, and probably more so. Azithromycin has a long half life (68 hours) with sub-MIC levels persisting for 2-4 weeks and probably longer intracellularly; the higher the total dose the longer the persistence of sub-MIC levels. BASHH took the pragmatic approach of increasing the total dose from 1.5 g but not to 2.5 g total used by Read et al which would be associated with a longer duration of intracellular sub-MIC levels (see BASHH Mgen guideline) and recommending no sexual intercourse with a new partner for 2 weeks after commencing therapy.
Treatment of Recurrent or Persistent NGU
If treated with doxycycline regimen first line:
Recommended
Azithromycin 1g stat then 500 mg once daily for the next 2 days, plus metronidazole 400mg twice daily for five days
Azithromycin should be started within 2 weeks of finishing doxycycline. This is not necessary if the person has tested Mgen-negative.
NB patients should be advised to abstain from sexual intercourse until 14 days after the start of treatment and until symptoms have resolved.* (see above)
If treated with azithromycin regimen first line:
Recommended
Moxifloxacin 400mg once daily for 10 days, plus metronidazole 400mg twice daily for five days
Alternative
Doxycycline 100mg twice daily for 7 days, plus metronidazole 400mg twice daily for five days**
**In the event of non-availability of Mgen detection assays, it may be reasonable to try this regimen before using moxifloxacin.2
Epidemiological Treatment
In the absence of MG testing, it is reasonable to provide epidemiological treatment to the partners of men with NGU using the same antimicrobial regimen that resulted in cure in the index case.
These recommendations are subject to change in light of new available evidence. We recommend that clinicians appraise and share data regarding NGU causes, treatment and outcomes to develop the evidence base in the UK.
2015 Guidelines FOR INFORMATION ONLY:
General advice
Full explanation of the diagnosis with written information should be provided including advice to abstain from sexual intercourse or if that is not acceptable consistent condom use including for oral sex until he and his partner(s) have completed treatment (IV,C).
Recommended regimens (A)
- Doxycycline 100 mg twice daily for 7 days (Ib)
or
-
Azithromycin 1 g stat (Ib)
or
-
If the patient (or their sexual partner) is known to be M. genitalium-positive: Azithromycin 500 mg stat then 250mg daily for the next 4 days (B, IIb)
Alternative regimens (A)
- Ofloxacin 200 mg twice daily, or 400 mg once daily, for 7 days (Ib)
or
- Azithromycin 500 mg stat then 250 mg daily for the next 4 days (see above) (B, IIb)
Sexual contacts
- Should be assessed and offered epidemiological treatment. The duration of ‘look back’ is arbitrary; 4 weeks is suggested for symptomatic men
- Women who are pregnant, at high risk of pregnancy or are breast feeding should be treated with azithromycin 1 g (IV, C)
Follow up
Indicated only if Chlamydia confirmed or persistent symptoms. Those remaining symptomatic should return to clinic and retreated appropriately and assessed for risk of re-infection (IV,C).
Persistent and recurrent NGU
- Persistent NGU occurs in 15-25% following initial treatment of acute NGU
- Recurrent NGU is recurrence of symptomatic urethritis occurring 30-90 days following treatment of acute NGU and occurs in 10-20%
- Any treatment of persistent NGU should cover M. genitalium and T. vaginalis and/or bacterial vaginosis- associated bacteria
- It is likely that re-treatment of the sexual partner and index case will be beneficial if persistent/recurrent NGU in the index case resolves follow- ing extended therapy but subsequently recurs. It would be sensible to use the extended regimen demonstrated to be effective unless contraindicated (IV, C)
- Trichomonas vaginalis and M. genitalium testing should be considered
Preferred regimen
- Azithromycin 500 mg stat then 250 mg daily for the next 4 days (III, B) plus Metronidazole 400mg twice daily for 5 days (IV, C)
- NB Azithromycin is now cheaper than when this regimen was first introduced and a higher dose regimen of azithromycin 1g stat then 500mg for the next 4 days could be considered (IV, C).
- This regimen is unlikely to be effective in cases of macrolide resistant M.genitalium.
Alternative regimen
- Moxifloxacin 400mg orally once daily for 10–14 days (IIIb, B) plus Metronidazole 400mg twice daily for 5 days (IV, C).
- This regime may be used in patients considered at risk of M.genitalium which is macrolide resistant; it should not be a preferred therapy due to risks including increased risk of life-threatening liver reactions (IV, C).
Continuing symptoms (limited evidence)
- Moxifloxacin 400 mg orally once daily 7-14 days (IIIb, B)
Consider quinolone antimicrobial resistance as a cause of treatment failure in men who remain M. genitalium-positive after treatment with moxifloxacin. At present no registered antibiotics are available for treatment. Pristinamycin is registered in France and may be effective in most cases.
- Urological investigation is usually normal unless the patient has urinary flow problems and is not recommended (IV, C)
- Consider other differential diagnoses e.g. chronic abacterial prostatitis, the chronic pelvic pain syndrome and psychosexual causes
- If a man with chronic NGU is cured post extended therapy but relapses following sexual intercourse, retreatment of an appropriately treated sexual partner would be prudent (IV, C) with the same antibiotic regimen that was effective in the index
- Erythromycin 500mg four times daily for 3 weeks has been shown to be effective. Clarithromycin 500mg twice daily for 3 weeks may be an alternative (IV, C)
Download the Full Guidelines
Download the full guideline here.
UPDATE Dec 2018:
Please note, a revision to the Management section was approved in December 2018. Details can be found in the Management section above, or here. The published guideline accessed above does not reflect the changes made in 2018.